Why Women’s Chronic Pain is Not Taken Seriously and Ways to Manage It
by Valerie Howes for You Are UnLtd:
Chronic pain can impact everything from your mood, to your sleep to your social life. “The first things we lose are fun activities and leisure and we end up only doing what we have to do,” says Sarah Sheffe, an occupational therapist at the Toronto Academic Pain Medicine Institute.
One in five Canadians experience chronic pain and the majority of sufferers are women. There are four women to every one man diagnosed with fibromyalgia. And as many as one in four women experience persistent pelvic pain – typically a more-bitter-than-sweet souvenir of pregnancy or childbirth.Studies also show that women experience pain both at a lower threshold and with more overwhelming intensity than men. Yet Sheffe says many female pain clients report they’re not taken seriously when they first consult their physician. Sound familiar?
“Many Female Pain Clients Report They’re Not Taken Seriously When They First Consult Their Physician.”
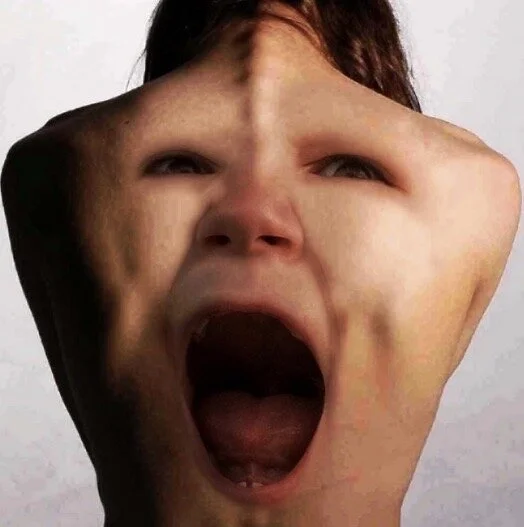
Beyond gender discrimination, part of the problem in diagnosing pain is that hundreds of regions of the brain are activated to interpret and communicate pain, and sometimes neural telephone tag ensues. You might not feel pain in the same part of the body that’s injured or inflamed. Or you may experience intense pain in relation to a seemingly minor physical issue. You could even hurt after an injury has healed, the most extreme example being the ‘phantom’ pain amputees report feeling in missing limbs.
Everything from your body chemistry to your lived experiences to your stress levels to your neural wiring can influence your subjective pain experiences. Sheffe makes this analogy: “When we hear an orchestra it’s the result of many instruments playing together; the output is beautiful music. The pain song is the output of many different parts of the brain. Our work is learning how to turn down the volume of the pain song and make it less disruptive.”
At MIND MATTERS: Women, Technology & Pain, held this summer at the University of Toronto, Sheffe joined forces with Babak Taati (assistant professor at Toronto Rehabilitation Institute) to share the latest science on how to make peace with pain. Taati’s research on the subject is supported by AGE-WELL, Canada’s technology and aging network, launched in 2015. The organization also co-hosts the MIND MATTERS series, along with Women’s Brain Health Initiative.
Take control
When pain becomes chronic (i.e., lasting longer than three months or beyond the expected healing period), it’s time to take your own healing in hand. “It’s empowering not to have to rely solely on healthcare providers,” says Sheffe.
Get temporary relief
Applying heat or cold or having a massage can create a different physical sensation that keeps your brain too busy to process pain – a welcome distraction. Medicinal creams and drugs, as recommended by your healthcare provider, can offer temporary relief too.
Retrain your brain
Mindfulness techniques, Qigong and deep breathing can all help reduce pain. The goal of acceptance and commitment therapy is to teach you how to shift your energies from trying to avoid suffering to making peace with whatever pain life presents and not letting it get in the way of living.
Gently challenge pain
Don’t give up and veg out! Keep moving and you’ll become fitter, stronger, healthier and more resilient. Set small goals that push you just outside your comfort zone. Yoga stretches can ache a little at first, but then they make you more flexible and mobile. Body mapping (understanding how the body parts fit together and function) helps you change how you move, so you can reclaim lost activities. And hydrotherapy may take self-steeling as you alternate between chilly and hot pools, but it also lowers blood pressure, improves blood flow and ultimately reduces pain.
Embrace tech
Both Sheffe and Taati are helping develop high-tech tools to change the pain game. Sheffe’s “I Can Cope” is an app in the research stage that allows patients to learn about their pain through mini lessons, practice and track management strategies, and connect in a virtual community. (While you’re waiting for this to hit the market, check out pain-tracking and -management apps, such as Curable, CatchMyPain and WebMD Mobile Pain Coach.)
Meanwhile, Taati is applying computer visioning to pain detection for older adults in long-term care facilities – 70 percent of whom are women. “Older adults are generally under-diagnosed and treated, especially if they have dementia or other conditions that interfere with verbal communication,” he says. His device detects facial expressions and movements that signal pain, then alerts care staff through a central computer system, so they can respond faster – a comfort to patients and their loved ones alike.